How Hospital Leaders Can Prepare for The Joint Commission’s Goal 12: Requirements, Strategy & Executive Checklist
 Bambi Gore
Bambi Gore

What Is Goal 12?
Beginning January 1, 2026, The Joint Commission will enforce National Patient Safety Goal 12: Health Professional Resource Management, a new national performance goal designed to ensure hospitals have competent, adequately staffed clinical teams aligned to patient needs. Goal 12 elevates staffing adequacy from an operational task to a core safety, quality and accreditation requirement, placing responsibility directly on hospital and health system leaders.
Why Goal 12 Matters to Hospital Executives
Goal 12 reflects what healthcare leaders already know:
- Staffing is not just a ratio question; it’s a patient safety issue.
- Workforce shortages, burnout, and turnover are affecting quality outcomes nationwide.
- Surveyors will now evaluate whether your staffing decisions are intentional, documented, competency-based, and tied to patient acuity.
Research across multiple studies links adequate RN staffing and skill-mix with:
- Lower mortality
- Fewer adverse events
- Reduced infections
- Shorter lengths of stay
Simply put: Goal 12 formalizes what patient safety science has already shown.
What Does Joint Commission Goal 12 Require?
Here are the core expectations, based on the official Joint Commission standard and supporting analysis:
- A defined staffing plan aligned to patient acuity and service complexity
Hospitals must show how staffing levels and skill-mix are determined and adjusted. - Verification of clinical competence for all caregivers
This includes:- Staff nurses
- Float pool clinicians
- Travelers and agency staff
- LPNs/UAPs providing delegated care
- A registered nurse available 24/7 to provide or supervise care
This RN oversight requirement aligns with CMS Conditions for Participation. - Leadership accountability for workforce planning and oversight
Nurse executives and hospital leaders must document their involvement in staffing decisions. - Documentation that supports staffing practice and decision-making
Hospitals must maintain evidence tracing how staffing decisions relate to patient needs, outcomes and unit conditions. - Escalation pathways when staffing falls below expectations
Organizations must define and activate contingency plans when staffing is insufficient.
A key clarification:
The Joint Commission is not setting fixed nurse-to-patient ratios. It is creating accountability systems that require hospitals to justify, document, and support how staffing decisions are made.
How to Prepare for Joint Commission Goal 12: Readiness Checklist for Executives
Here is an easy checklist designed to help you prepare for accreditation:
- Leadership & Governance
Ask: Do leaders have clear accountability for staffing oversight?
Actions:- Assign executive ownership (CNO, COO, or designee).
- Set quarterly reviews of staffing adequacy.
- Document governance structure.
- Staffing Plan & Skill-Mix Alignment
Ask: Is staffing tied to patient acuity, complexity and care models?
Actions:- Update acuity tools.
- Validate skill-mix appropriateness for each unit.
- Review high-variability units monthly.
- Competency Validation & Clinician Readiness
Ask: Are staff, float, and travelers competent for their assigned settings?
Actions:- Standardize competency checklists.
- Require unit-specific validations.
- Maintain accessible competency files for surveyors.
- Staffing Data, Outcomes & Documentation
Ask: Can your hospital show the relationship between staffing and patient outcomes
Actions:- Track staffing levels daily.
- Trend HAPIs, falls, infections, and other safety metrics.
- Tie data to staffing decisions.
- Escalation Policies
Ask: Are escalation protocols documented and consistently followed?
Actions:- Define contingency thresholds.
- Train charge nurses and supervisors on escalation workflow.
- Log variances and interventions.
- Staffing Agency & Vendor Alignment
Ask: Do external staffing partners meet your standards for competency and documentation?
Actions:- Update vendor expectations and contracts.
- Require transparency around credentialing.
- Conduct periodic audits of agency staff competency.
Download a copy of the Joint Commission Goal 12 Readiness Checklist.
Frequently Asked Questions (FAQs) About Joint Commission Goal 12
- What is Joint Commission Goal 12?
A national performance goal requiring hospitals to align staffing levels and competence with patient needs. - Does Goal 12 mandate nurse-to-patient ratios?
No. It requires hospitals to justify and document their staffing decisions based on acuity and complexity. - Who is responsible for Goal 12 compliance?
Hospital leadership is accountable, especially nursing and operational executives. - When does Goal 12 go into effect?
January 1, 2026. - What documentation will surveyors expect?
Staffing plans, competency validations, acuity data, and evidence of leadership oversight.
Key Takeaways for Healthcare Leaders
- Goal 12 represents a major shift toward accountable, competency-aligned staffing.
- It requires clear documentation, not predefined ratios.
- Leadership involvement is not optional; it’s an accreditation expectation.
- Data-driven workforce planning is now fundamental to patient safety, compliance, and operational performance.
- Hospitals that prepare proactively will be positioned to demonstrate value, reduce risk, and improve outcomes.
How Trio Workforce Solutions Supports Goal 12 Readiness
As hospitals prepare for the implementation of The Joint Commission’s Goal 12, many leaders are reassessing their current workforce partners and find that these partners are not prepared to provide the competency validation, documentation accuracy, and staffing alignment that this new performance standard requires. Trio Workforce Solutions was built with this level of rigor in mind.
Our model is designed to meet the needs of healthcare organizations facing increased accountability for staffing decisions, skill-mix, and clinician competence. We align our processes directly with TJC, DNV, and CMS requirements, ensuring hospital leaders can demonstrate continuous readiness, not just during a survey, but every day.
- Compliance Built for Accreditation-Level Expectations
Trio’s credentialing and compliance workflows are structured to support the detailed documentation required under Goal 12, including:- Primary source verification for all licenses, certifications, and education
- Real-time monitoring of sanctions, exclusions, and expirables
- Facility- and unit-specific alignment of credentialing checklists
- Ongoing audits and quality checks to ensure files remain current and survey-ready
- Clinical Oversight That Aligns Competency With Patient Needs
Our clinical team, led by an experienced nurse executive, works directly with our compliance specialists to ensure each contingent clinician is competent for the specific unit and care environment where they will practice.
This includes:- Validation of unit-specific competencies
- Scope-of-practice alignment
- Clinical readiness assessments before assignment
- Continuous collaboration to support high-reliability workforce planning
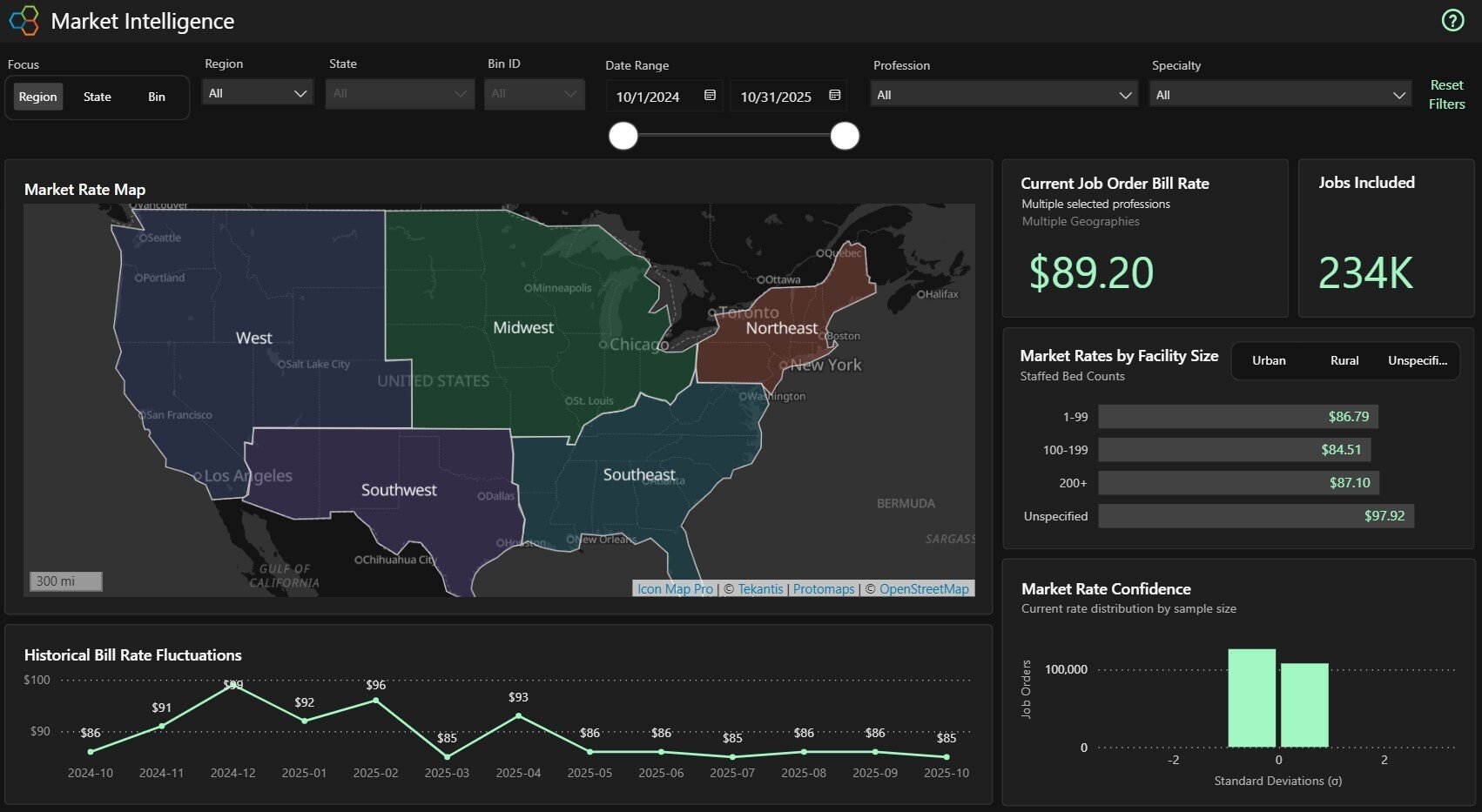
- Transparent, Actionable Workforce Intelligence
Trio provides dashboards, reporting tools, and documentation summaries that help hospital executives quickly demonstrate alignment between staffing decisions, acuity, and patient care needs.
This includes:- Compliance status dashboards
- File verification and expiration summaries
- Unit-specific competency tracking
- Data to support leadership accountability and decision-making
- A Partner in Continuous Readiness
Goal 12 shifts workforce strategy from a reactive operational function to an ongoing executive responsibility. Trio supports this shift by providing:
- Proactive monitoring
- Predictive compliance alerts
- Documentation that is always survey-ready
- Clinical and compliance support during on-site or virtual survey activities
- Supporting Hospitals Through Every Step of Workforce Transformation
As staffing expectations evolve, Trio Workforce Solutions stands alongside healthcare leaders to help build workforce strategies that are:- Safe
- Transparent
- Accreditation-aligned
- Clinically appropriate
- Operationally sound
Whether you are preparing for Goal 12, navigating a TJC or DNV survey, or reassessing your workforce model, Trio provides the structure, oversight, and collaboration hospital leaders need to remain confident in their staffing approach.